Bioprinting Innovative 3D Cellular Models to Test New Therapies for Hereditary Eye Disease
SECTION: OPHTHALMOGENETICS
For genetic eye disorders, numerous potential therapies are currently under development, including gene-, small molecule-, and cell replacement (transplantation)- therapy. Recently, the first genetic therapy for the orphan disease RPE65-genotype retinitis pigmentosa has hit the market. Amsterdam UMC is one of the first treatment centers for this therapy.

However, there is an unmet need in the field for human cell models representative of genetic disease to pre-clinically test these new therapies. One highly innovative way to construct next-generation human cell models is 3D cellular bioprinting. The Department of Human Genetic’s Ophthalmogenetics section’s Bioprint Group recently installed a state-of-the-art 3D cellular bioprinter.
This bioprinter can, via computerized design, print living cells and extracellular matrix with an unprecedented resolution of 2 micrometer.
In 2021, the Bioprint Group successfully bio-printed the first proof-of-concept in vitro model for Age-related Macular Degeneration (AMD), a frequent and devastating blinding disease.
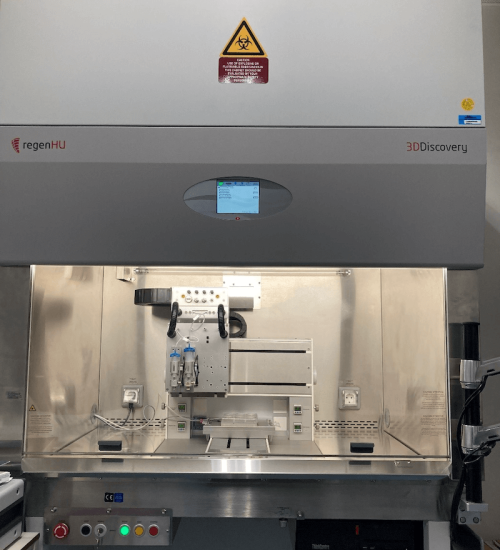
Front view of the 3D cellular bioprinter. In the middle, top: the high precision bioprinter robot arms set-up in an ultra-clean flow cabinet.
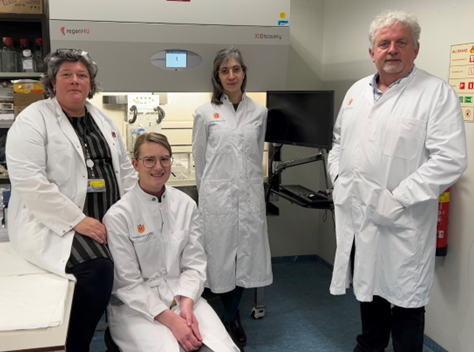
The Human Genetics Department, Ophthalmogenetics Section Bioprint Group in front of the new 3D cellular bioprinter. From Left to Right: Jacoline ten Brink (Senior Operator), Roos Sanne Verkerk (Junior Operator), Dr. Eszter Emri (post-doc and chief daily operations), and Prof. Arthur Bergen (Head of the Section and co-initiator). Members of the group not in this picture: Prof. Theo Smit (Department of Medical Biology and co-initiator) and Prof. Huveneers (Department of Medical Biochemistry; cardiovascular angle).
AMD is complex disorder caused by environmental and genetic factors. Until now, there was not a good pre-clinical model representative of the disease that could be used to test new therapies. The new bioprinted in vitro model for AMD consists of a basement membrane with human stem-cell derived, genetically defined neural pigment epithelial (RPE) cells on top. In between these layers, the group has printed highly defined deposits (drusen; plaques) that are the hallmark of early-stage AMD.
The computerized design of this bioprinted model can also be adapted for a number of other monogenic or complex disorders, including gyrate atrophy, ocular albinism, RPE-related retinitis pigmentosa, atherosclerosis, and Alzheimer disease (plaques).